Find an MPOX Vaccine Near You
Visit Empowered Against MPOX to find one!
California State University, San Bernardino
5500 University Pkwy, San Bernardino, CA 92407
Last Thursday of each month
from 11am – 2:30 pm
San Bernardino Valley College
701 South Mount Vernon Avenue, San Bernardino, CA 92410
First Wednesday of each month from 10am -1pm
Hesperia Health Center
16453 Bear Valley Rd
Hesperia, CA 92345
Every Thursday
AIDS Healthcare Foundation
8263 Grove Ave, Rancho Cucamonga, CA 91730
Second Wednesday of each month from 11:30 am-2:30 pm
Ontario Health Center
150 E. Holt Blvd.
Ontario, CA 91761
Every Monday
San Bernardino Health Center
590 N. D St.
San Bernardino, CA 92401
Every Friday
What is mpox?
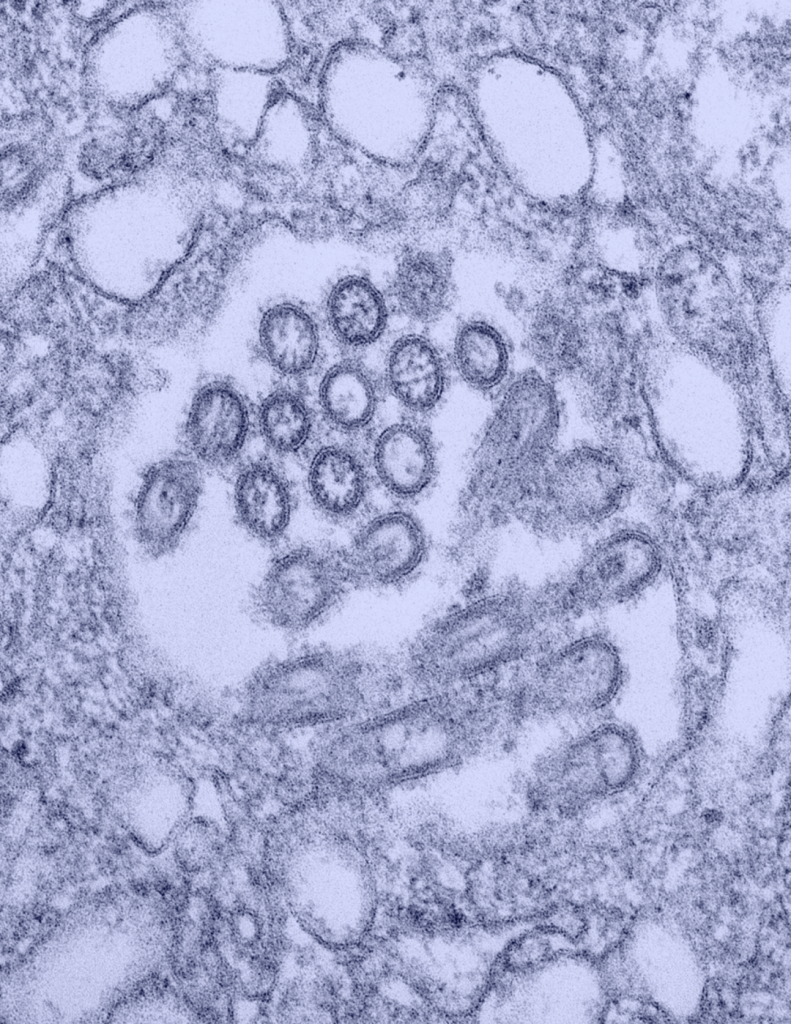
Mpox (formally known as monkeypox) is a rare disease caused by the mpox virus. The mpox virus is part of the same family of viruses as the variola virus, which causes smallpox. Mpox is a public health concern because the illness is similar to smallpox and can be spread from infected humans, animals, and materials contaminated with the virus. There are no known cases in the US of animals spreading the virus. Current animal cases are in central and west Africa from rodents and primates that can spread the virus. Household pets are not an issue. Mpox is less transmissible and usually less severe than smallpox.
Mpox was first identified in 1958 and occurs primarily in Central and West African countries. Historically mpox cases have occurred in the U.S. rarely and mostly related to international travel or importation of animals. Since 2022, there has been a recent significant increase in reported cases where mpox is not commonly seen, including in Europe, Canada, the United States, and California. While it’s good to stay alert about emerging public health outbreaks, the current risk of getting mpox in the general public is very low.
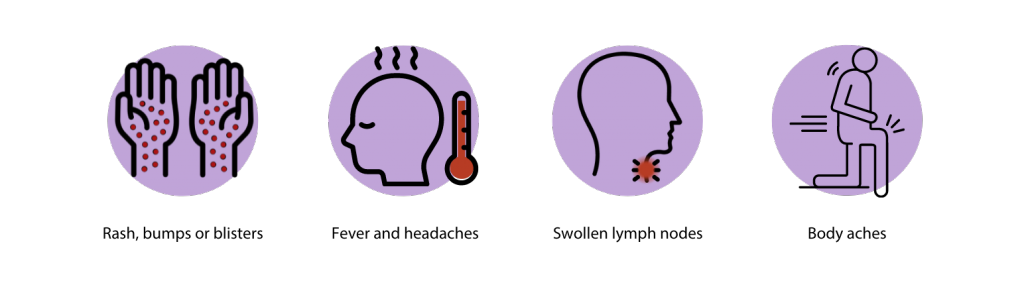
Mpox Symptoms
Individuals with mpox may experience a range of symptoms, which can vary in severity. Initially, mpox may manifest with flu-like symptoms such as fever, fatigue, swollen lymph nodes, and body aches. Typically within 1 to 3 days, although occasionally taking longer, after the onset of fever, a rash or sores may appear. These can resemble pimples or blisters and may cause discomfort and itching.
The rash or sores might appear in the genital region (including the penis, testicles, labia, and vagina) or around the anus, but they can also manifest on other parts of the body such as the hands, feet, chest, and face. They may also be limited to one part of the body.
The sores will go through several stages, including scabs, before healing.
The sores progress through various stages, including scabbing, before eventually healing. The majority of individuals with mpox will develop a rash or sores, although some may experience these symptoms before or without the presence of flu-like symptoms. Mpox is contagious from the onset of symptoms until all sores have completely healed and a new layer of skin has formed, typically lasting 2-4 weeks.
Isolation
A person with mpox can spread it to others from the start of symptoms until all sores have healed, scabs have fallen off, and a fresh layer of skin has formed underneath, which can take several weeks. There is a growing body of scientific evidence that shows some people can spread mpox virus to others from 1 to 4 days before symptoms appear.
If you were exposed or experience mpox symptoms, seek medical care for further testing and stay away from others.
Ensure to wear a mask and cover your rashes or sores when seeking medical attention. For full isolation guidance, consider the following: CDC Mpox Isolation Recommendations.
How does mpox spread?
Mpox can spread through direct contact with an infected person or their body fluids. Activities include:
- Direct contact with the infectious rash, scabs, or body fluids
- Prolonged, face-to-face contact
- Intimate physical contact, such as kissing, cuddling, or sex
- Touching items (such as clothing, linens, and utensils) that previously touched the infectious rash or body fluids
- Being scratched or bitten by an infected animal
- Using products from an infected animal
- Pregnant people can spread the virus to their fetus through the placenta
When can a person spread mpox?
Mpox can spread from the time symptoms start until the rash has fully healed and a fresh layer of skin has formed. It is currently unclear if people who never had symptoms have spread the virus to someone else.
Is my child at risk for mpox?
The likelihood of your child getting mpox is very low; however, the CDC has detailed recommendations for Schools, Early Care and Education Programs, and Other Settings Serving Children or Adolescents.
A general overview of frequently asked questions regarding your child or adolescent and mpox are described below:
Settings should follow their everyday operational guidance that reduces the transmission of infectious diseases.
- Stay home when sick
- Identify private spaces to keep ill child away from others
- Wash hands with soap and water
- Clean and disinfect
- Wear personal protective equipment (PPE) are recommended for staff taking care of infected students
If there is a mpox exposure, the department of health will help in considering appropriate actions to prevent the spread of the virus.
At this time, CDC recommends vaccination for people who have been exposed to mpox and people who may be more likely to get mpox, including:
- People who have been identified by public health officials as a contact of someone with mpox
- People who know one of their sexual partners in the past 2 weeks has been diagnosed with mpox
- People who had multiple sexual partners in the past 2 weeks in an area with known mpox
At this time, there is no need for widespread vaccination for mpox among children or staff at K-12 schools or early childhood settings. For more information on vaccination against mpox, see these answers to frequently asked questions about vaccination.
Currently, the risk of mpox to children and adolescents is low. Several illnesses can cause a rash and fever in children, such as hand-foot-mouth disease and chickenpox (varicella). For a child without a known exposure to mpox, a fever and rash should be evaluated by a medical professional and settings should follow their standard illness policies for these situations. A healthcare provider can determine what treatment or testing the child needs. It is important to avoid stigma.
There are also multiple potential causes of rashes in adults. Parents, teachers, and staff members should understand the symptoms of mpox and see a healthcare provider if they remain concerned. Adults with symptoms of mpox should also:
- Avoid close contact, including sex or being intimate with anyone, until they have been checked out by a healthcare provider.
- Visit a public health clinic near them if they don’t have a provider or health insurance.
- Wear a well-fitting mask when they see a healthcare provider.
The department of health will provide guidance for people exposed to mpox on how to monitor for symptoms. If a rash develops, an individual should follow isolation and prevention practices until (1) the rash can be evaluated by a healthcare provider, (2) testing is performed, if recommended by the healthcare provider, and (3) results of testing are available and are negative.
- Children and adolescents who are exposed to mpox should be monitored for symptoms for 21 days.
- Some symptoms in young children may be difficult to recognize promptly. When monitoring a child for illness following exposure to mpox, parents and caregivers should check the child’s temperature daily. Parents and caregivers should also perform daily full-body skin checks for a new rash and inspect the inside of the mouth for any sores or ulcers on young children.
- In older children and adolescents, parents can help with the inspection of the mouth and exposed skin areas that may be difficult for the child or adolescent to see (back of neck, arms, legs). They can also remind the child and adolescent to be aware of any rash or pain in areas covered by clothing, including the genitals, and to inspect those areas for rash and let the parent know if they notice any changes in their skin or feel any pain in those areas.
- If a child or adolescent develops symptoms while at home, the parent or caregiver should contact the local health department and their healthcare provider. The child should not return to the educational setting until medically assessed.
- Ideally, another adult in the household without mpox should serve as primary caregiver, when possible.
- If a child cannot be completely separated from the parent or caregiver with mpox, the parent or caregiver should continue to care for the child in an age-appropriate manner including regular interaction based on the physical and emotional needs of the child.
- During interactions, the parent or caregiver should cover their rash with clothing, gloves, or bandages, wear a well-fitting mask, and follow other prevention practices.
- The child or adolescent, if 2 years of age or older, should wear a well-fitting mask or respirator during interactions with the parent or caregiver.
- The guidance for Disinfecting the Home and Other Non-Healthcare Settings to clean and disinfect surfaces, floors, and shared items used by the person with mpox should be followed.
- The parent should work with their doctor and their health department for further guidance on the child’s activities outside the home.
- It is also important to discuss vaccination for exposed children with the health department. A vaccine is available that can help prevent mpox in people who have been exposed if it is given soon after exposure.
Prevention
There are various ways to prevent getting infected with mpox:
- Getting vaccinated (two-doses) for mpox
- Continue to reduce behaviors that increase risk of mpox until 14 days after the 2nd dose
- Communicate with sexual partners about recent illness or unexplained sores or rashes on the body
- Avoid close contact, including hugging, cuddling, and sex with people with symptoms
- Wash your hands often with soap and water or use an alcohol-based hand sanitizer
- Wear appropriate PPE (mask, gown, gloves) when caring for people with mpox
- When traveling to countries where mpox is present, avoid contact with animals that can spread mpox virus, usually rodents and primates. Also, avoid sick or dead animals, as well as bedding or other materials they have touched.
Talk to your doctor if:
- You believe you were exposed to mpox or develop symptoms of fever, swollen lymph nodes or pimple-like rash/blister.
Vaccination
Get vaccinated if you are at risk for mpox; the vaccine will help prevent serious illness two weeks after the second dose. Any person who MAY be at risk for mpox infection or persons who request vaccination may receive the vaccination without having to report specific risk factors.
- Visit the CDPH Vaccine Page to learn more about the JYNNEOS vaccine.
- Visit MyTurn.Ca.Gov to schedule an appointment
How to get tested for mpox?
If you think you have mpox based on the symptoms shown above or if you have been in contact with someone who has mpox, it is important to get in touch with your healthcare provider so they get you tested.
Treatment
Most mpox infections may be mild and heal without additional treatment. However, anti-viral drugs, such as terovirimat (TROXX) may be used to treat mpox. It is usually recommended for people who are experiencing severe symptoms and illness or are at high risk.
High-risk groups include weakened immune systems, young children less than 1 year of age, and those who are pregnant. If you are interested in treatment, reach out to your healthcare provider or a local clinic.
More information can be found in the CDC’s Patient’s guide to TPOXX.