Emerging Diseases
Candida auris
Candida aurisis a fungus that causes serious infections and spreads in healthcare facilities. Infection preventionists, healthcare personnel, and laboratory staff can all help prevent it from spreading.
Why is Candida auris a problem?
- It causes serious infections. C. auris can cause bloodstream and other types of invasive infections, particularly in patients in hospitals and nursing homes who have many medical problems. More than 1 in 3 patients die within a month of being diagnosed with an invasive C. auris infection.
- It is often multidrug-resistant. Antifungal medications commonly used to treat other Candida infections often don’t work for C. auris. Some C. auris isolates are resistant to all three major classes of antifungal medications.
- It is becoming more common. Although C. auris was just discovered in 2009, the number of cases has grown quickly. Since 2009, it has been reported in dozens of countries, including the United States.
- It is difficult to identify. C. auris can be misidentified as other types of fungus unless specialized laboratory methods are used. Correctly identifying C. auris is critical for starting measures to stop its spread and prevent outbreaks.
- It can spread and cause outbreaks in healthcare facilities. Just like other multidrug-resistant organisms such as carbapenem-resistant Enterobacteriaceae (CRE) and methicillin-resistant Staphylococcus aureus (MRSA), C. auris can be transmitted in healthcare settings and cause outbreaks. It can colonize patients for many months, persist in the environment, and withstand some commonly used healthcare facility disinfectants.
Early detection and infection control can limit the spread of C. auris.
Prepare for C. auris in your facility
- Work with your laboratory to ensure the fungus identification method used in your facility can identify C. auris. If it cannot, know when to suspect C. auris and send suspected isolates to your state or local public health department for further identification.
- Begin surveillance. Establish a protocol with your laboratory so that your department is promptly informed when C. auris is suspected.
- If your laboratory is not equipped to identify C. auris, begin surveillance for the organisms that commonly represent a C. auris misidentification. See https://www.cdc.gov/fungal/candida-auris/recommendations for common misidentifications by different yeast identification methods.
- Know which patients are at higher risk for C. auris infection or asymptomatic colonization. These include:
- Patients who have received healthcare in post-acute care facilities (e.g., nursing homes), especially those with ventilator units.
- Patients recently hospitalized outside the United States, especially in countries with known C. auris cases (visit www.cdc.gov/fungal/candida-auris for a map of countries), and patients infected or colonized with carbapenemase-producing bacteria.
- Have a response plan. Discuss recommendations for infection prevention and control of C. auris with healthcare personnel, including environmental services.
What should I do if there is C. auris in my facility?
- Check the CDC website for the most up-to-date guidance on identifying and managing auris: www.cdc.gov/fungal/candida-auris.
- Report possible or confirmed auris test results immediately to your public health department.
- Ensure adherence to CDC recommendations for infection control, including
- Placing patients infected or colonized with C. auris on Transmission-Based Precautions and, whenever possible, in a single room.
- Making sure gown and gloves are accessible and used appropriately.
- Reinforcing hand hygiene.
- Coordinate with environmental services to monitor and ensure the patient care environment is cleaned using a disinfectant with an Environmental Protection Agency claim for C. auris or, if not available, for Clostridioides difficile. These products can be found at www.cdc.gov/fungal/candida-auris/c-auris-infection-control.html. Some disinfectants used in healthcare facilities (e.g., quaternary ammonium compounds [QACs]) may not be effective against C. auris, despite claims about effectiveness against C. albicans or other fungi. Work with the environmental services team to monitor the cleaning process.
- After consulting with public health personnel, screen contacts of case-patients to identify patients with auris colonization. Use the same infection control measures for patients found to be colonized.
- When a patient is being transferred from your facility (e.g., to a nursing home or other hospital), clearly communicate the patient’s auris status to receiving healthcare providers.
COVID-19
2019 Novel Coronavirus (COVID-19, formerly known as 2019-nCoV) is a virus that has been identified as the cause of an outbreak of respiratory illness. Initially it was thought to be animal-to-person transmission, due to the majority of the infected being linked to the animal and seafood market. However, after a growing number of patients having no ties to these markets, it is indicated that person-to-person transmission is occurring. It is unclear at this time how easily the virus is being spread between people. For the most recent situation summaries and updates please visit the Centers for Disease Control and Prevention web page.
Symptoms and Complications
The symptoms of COVID-19 infection range from little to no symptoms, to individuals being severely ill and dying. Some symptoms of COVID-19 include, but are not limited to:
- Fever
- Cough
- Shortness of breath
Currently the CDC believes that symptoms appear in as little as 2 days or as long as 14 days after being exposed. These times are based off of the previous incubation period of MERS viruses.
Transmission
Coronaviruses come from a large family of viruses that are commonly found in different animal species such as camels, cattle, cats, and bats. It is rare for a coronavirus to infect a person, and then spread from that person to another person, such as cases of MERS and SARS.
In the case of person-to-person transmission it is thought to have been transferred via respiratory droplets that are emitted into the air when an infected individuals coughs or sneezes. This is similar to how influenza and other respiratory illnesses are spread. It is important to look at how easily a virus is able to be spread from person-to-person. Some viruses are extremely contagious, such as measles, while others are much less contagious. COVID-19 is being considered a serious public health threat by the CDC, however, based on the current information, the immediate health risk to the general public in America is considered low for the time being.
Prevention and Treatment
Currently there is no vaccine to prevent COVID-19. The best prevention is avoiding the virus as much as possible. The CDC also always recommends everyday preventative measures be taken to help prevent the virus being spread. These measures include:
- Hand washing often with soap and water for no less than 20 seconds.
- If access to soap and water is not available, the use of alcohol base sanitizer is recommended.
- Avoid touching your eyes, nose, and mouth without first washing your hands.
- Avoid contact with sick individuals
- Stay home if you are sick
- Cover your cough or sneeze with a tissue, then immediately dispose of the tissue in the trash.
- Clean and disinfect surfaces and objects that are frequently touched as much as possible.
By having these everyday habits you can help to prevent the spread of several different viruses, including COVID-19.
Tuberculosis Prevention and Care
The Tuberculosis Control Program performs disease detection, surveillance, case management, and investigatory activities designed to control the incidence of tuberculosis (TB) in the County. The program provides tuberculosis information and educational resources for the Department, medical community, and general public. Please call (800) 722-4794 to speak to a TB staff member.
Nationwide Drug Shortage
To obtain up to date information regarding the status of the shortage please visit the FDA’s Center for Biologics Evaluation and Research-Regulated Products website listed below. https://www.fda.gov/vaccines-blood-biologics/safety-availability-biologics/cber-regulated-products-current-shortages
The following link outlines the CDC’s recommendations for dealing with the reduction in TB testing capability. https://www.cdc.gov/mmwr/volumes/68/wr/mm6824a4.htm
Clinical Services Offered
Skin testing for tuberculosis is offered at Department of Public Health clinics throughout the County. For more information. Please call (800) 722-4777 for an appointment and information on clinic locations and times.
Basic TB Facts
- Q: What is TB?
A: Tuberculosis (TB) is a disease caused by germs that are spread from person to person through the air. - Q: How is TB spread?
A: TB germs are put into the air when a person with TB disease in the lungs or throat coughs, sneezes, speaks, or sings. These germs can stay in the air for several hours, depending on the environment. People who breathe in the air containing these TB germs can become infected. - Q: What is a latent TB infection?
A: People with latent TB infection have TB germs in their bodies, but they are not sick because the germs are not active. These people do not have symptoms of TB disease and they cannot spread the germs to others. However, they may develop TB disease in the future. - Q: How do you know if you have latent TB?
A: A TB skin test is used to test for latent TB. - Q: Treatment
A: Both latent TB infection and TB disease can be treated with medication.
Per Health and Safety Code Section 120175, local health departments as designated by the Health Officer are responsible for preventing the spread of tuberculosis within their jurisdictions. They are granted the authority to take the necessary measures to prevent the spread. When care is not provided by the department of public health TB Controller, the local health department tuberculosis program will oversee a case. View the Guidelines for Oversight of Tuberculosis Care. For information you can also visit the Current CDPH-CTCA Joint Guidelines website.
The Tuberculosis Control Program offers case management services to all patients with active TB disease. A TB clinician and controller is also available to answer any questions regarding the medical management of your patient. Call 800-722-4794 to speak to a TB clinician and controller.
The Tuberculosis Control Program also offers directly observed therapy (DOT) to patients who meet certain criteria. Please read the Guidelines for DOT for information on eligibility criteria.
Report a Case of Tuberculosis
Health care providers must report suspected or confirmed cases of TB to the Tuberculosis Control Program. Please fill out a TB Health Facility Discharge Planning Guidelines for your hospitalized or clinic patient and fax to (909) 381-8471. Follow up with a phone call to one of our TB nurses at (800) 722-4794.
TB Health Facility Discharge Planning Guidelines
Reporting Tuberculosis Infection Using Skin Tuberculin Test or IGRA
Health care providers can submit a report of a TB infection, such as a positive skin tuberculin test or interferon-Gamma Release Assay (IGRA) (i.e. QuatiFERON Gold), using a Confidential Morbidity Report (CMR). This form is only to be used to report a positive tuberculin skin test or IGRA.
Any active or suspect cases must be made using the forms outlined in “Report a Case of Tuberculosis” section. These types of cases will not be accepted on a CMR form.
The Centers for Disease Control and Prevention (CDC) revised the Tuberculosis (TB) Technical Instructions for Civil Surgeons. These instructions went into effect on October 1, 2018. These instructions now require that civil surgeons report all persons diagnosed with latent TB infection (LTBI) to the local health department where the applicant resides. These new requirements also include the use of a TB blood test [interferon-gamma release assay (IGRA)] instead of a tuberculin skin test (TST) for TB screening of applicants’ ≥ 2 years old.
Civil surgeons are also required to refer all applicants whose CXR findings are suggestive of TB disease, all applicants with symptoms or signs of TB disease, all applicants with known HIV infection, and all applicants with extrapulmonary TB to the local health department for further evaluation.
To report LTBI using the CMR
To report TB disease or suggestive TB disease use the: Initial TB Case Report Form

TB-related Resources
Guidelines for Treatment:California Tuberculosis Controllers Association
TB Training & Educational Resources:Curry International TB Center
Find an FQHC clinic for TB services click here
Latent TB Infection (LTBI) ResourcesProvider Fact Sheet- Window Prophylaxis
Syphilis
Syphilis is a sexually transmitted disease (STD) caused by bacteria (germs). Syphilis is easy to cure. Without treatment, it can hurt your body’s organs. Congenital syphilis is when a pregnant woman passes syphilis to her baby during pregnancy or childbirth. It can cause a woman to have a baby too early or cause a miscarriage or stillbirth (a baby born dead). It can also lead to serious health problems in babies.
Symptoms
Often people don’t notice symptoms, so they don’t know they’re infected. Signs of syphilis may include a sore near the area where the germ entered the body (vagina, anus, lips, or mouth) or rash on one or more areas of the body. The symptoms may appear and disappear. The only way to know for sure is to get tested.
Transmission
You can get syphilis by having contact with a syphilis sore during vaginal, anal, or oral sex. Sores can be found on the penis, vagina, anus, or on the lips and mouth. You may not see the sores and they don’t cause pain. Congenital syphilis spreads from mother to baby during pregnancy or birth.
Treatment
Syphilis can be treated and cured with antibiotics (medicine that kills germs). Make sure your sex partner(s) get tested and treated too. This will help them stay healthy, avoid infecting others, and avoid re-infecting you.
Prevention and Testing
- Use condoms.
- Go to your doctor for testing and treatment as early as possible.
If you don’t have a regular doctor, call (800) 722-4777 to make an appointment for clinic services at San Bernardino County clinics. Test if you are experiencing symptoms. Test if you are getting tested for other STDs. If you are having sex without using a condom and/or have multiple sex partners, get tested every 6 months. If you are a man having sex with other men, get tested every 3-6 months. Test if you are a woman and plan to get pregnant. If you’re pregnant, remind your doctor to test you three times: during your first trimester (1 – 12 weeks), third trimester (28 – 32 weeks), and at delivery.
Measles
What Is Measles?
Measles is an acute, highly contagious viral disease. Symptoms include a high fever, runny nose (coryza), cough, loss of appetite, a rash, and red, watery eyes (conjunctivitis). The rash usually lasts 5–6 days, begins at the hairline, moves to the face and upper neck, and proceeds down the body.
How Long Does It Take to Show Signs of Measles After Being Exposed?
It takes an average of 7-14 days from exposure to the first symptom, which is usually fever. The measles rash appears approximately 14 days after exposure, usually 2–3 days after the fever begins.
What Should Be Done If Someone Is Exposed to Measles?
Notification of the exposure should be communicated to a doctor. If the person exposed has not been vaccinated, measles vaccine may prevent disease if given within 72 hours of exposure. Immune globulin (a blood product containing antibodies to the measles virus) may prevent or lessen the severity of measles if given within six days of exposure.
How Can Measles Be Prevented?
There is a vaccine available to prevent measles. Vaccines are available from your medical provider or the San Bernardino County Department of Public Health clinics. View the Public Health’s Clinic Locations webpage for information about clinic locations and times or call the Communicable Disease Section at 1 (800) 722-4794, Monday through Friday, from 8 a.m. to 5 p.m. to find a location near you. For more information, view the California Department of Public Health measles website.
School Resource Corner
- Be Ready for Measles Toolkit – CDC’s preparedness and outbreak response tool for communication.
- Template Measles Email Communication for Schools
- Communication Toolkit – California Department of Public Health (CDPH)
- Q&A for MMR – My Turn: California Vaccine Site
- Immunization Timing Block Schedule – English | Spanish
- CDC Measles Toolkit for Schools and Childcare Settings – Includes fact sheets, notification templates, and social media graphics.
- Don’t Wait – Vaccinate! Toolkit – CDPH
- Visiting Another Country? Think Measles – Poster in multiple languages

Measles-related Resources
News Release: First confirmed measles case in San Bernardino County released 2/6/26
Measles Investigation Quick Sheet – California Department of Public Health
Public Health Laboratory – Measles Test Guidance
Health Advisory 2/4/26 – California Department of Public Health
Measles Information – California Department of Public Health
Should I Test For Measles? – Flowchart
Summary of Current Recommendations on Measles Immunization
Measles Clinical Guidance: Identification and Testing of Suspect Measles Cases
Measles Isn’t Just a Little Rash Infographic – English | Spanish
Hepatitis A – Related Resources
Hepatitis A – Guidelines for Disinfection
Hepatitis A – February 6, 2020 Outbreak News Release
Health Advisory – Hepatitis A Prevention and Recommendations
Hepatitis A
What is hepatitis A?
Hepatitis A (hep A) is a highly contagious liver infection caused by the hepatitis A virus (HAV). The mode of transmission for HAV is through the fecal-oral route and can be easily spread when consuming food, drinking water, or touching an object contaminated with fecal matter. Hepatitis A does not usually cause long-term liver damage. However, in rare cases, it can lead to a sudden loss of liver function.
Symptoms of hep A include fatigue, nausea and vomiting, abdominal pain or discomfort, clay-colored bowel movements, loss of appetite, dark urine, joint pain, yellowing of the skin and white of your eyes (jaundice), and intense itching. They generally do not appear until a person has had the infection for a few weeks.
Unvaccinated individuals are at highest risk.
Individuals who are unvaccinated against hep A, those who travel to or live in countries where hep A is common, msm (men who have sex with men) individuals, the homeless, IV drug users, household members or caregivers of a person with hep A, and those with clotting factor disorders are at highest risk of hep A.
While hep A is highly contagious, it is easily preventable by getting the hep A vaccine.

Zika-related Resources
Zika Information – California Department of Public Health (CDPH)
Non-native Mosquito Species – California Department of Public Health (CDPH)
Centers for Disease Control (CDC) on Zika
Mosquitos and Vector Control Program – San Bernardino County Department of Public Health (SBCDPH)
Zika
What Is the Zika Virus?
Zika virus is a mosquito-borne virus that prior to 2015 occurred in Africa, Southeast Asia, and the Pacific Islands. However, in May 2015, the Pan American Health Organization (PAHO) issued an alert about the first confirmed Zika virus infections in Brazil. Since then Zika virus has been identified in several countries throughout South and Central America, and the Caribbean. There are currently no local detections of the Zika virus in San Bernardino County. For up-to-date information on where Zika is locally transmitted, please view the Centers for Disease Control and Prevention website.
Most people infected with Zika virus will not develop symptoms. If symptoms do develop, they are usually mild and include fever, joint pain, rash and eye redness. If you have returned from an affected country and have any of these symptoms within two weeks, or any other symptoms following your return, please contact your medical provider and tell the doctor where you have traveled. While there is no specific treatment for the Zika virus disease, the best recommendations are supportive care, rest, fluids and fever relief.
How Is It Spread?
Zika virus is spread by the bite of an infected Aedes species mosquito, which actively bite humans during the daytime. These are the same mosquitoes that spread dengue, chikungunya, and yellow fever viruses. Mosquitoes become infected when they feed on a person already infected with the virus. Infected mosquitoes can then spread the virus to other people through bites. Zika virus is rarely spread from person to person. There have been rare instances of sexual and perinatal (mother-to-child) transmission, as well as through blood transfusion.
What Are the Symptoms?
Although most people who become infected with Zika virus have no symptoms, approximately 20% may develop acute onset of fever with rash, joint pain, or conjunctivitis (red eyes). Symptoms begin between 2 and 12 days (most commonly 3-7 days) after exposure to the virus. Other commonly reported symptoms include muscle aches and headache that may last for several days to a week. Severe disease requiring hospitalization is uncommon and deaths from the disease are rare. However, there have been cases of Guillain-Barré syndrome reported in patients following suspected Zika virus infection.
Pregnancy and Zika
The Zika virus can cause birth defects in pregnant women. Researchers have amassed enough evidence to conclude that Zika infection during pregnancy is a cause of microcephaly (abnormal brain and small heads) and other severe fetal brain defects.
Zika and Pregnancy Poster
Zika y Embarazo
What Can You Do?
Residents can still take precautions to avoid mosquito breeding areas around their homes by following these tips.
- Drain or Dump – Remove all standing water around your property where mosquitos lay eggs such as birdbaths, old tires, pet watering dishes, buckets, or even clogged gutters.
- Clean and scrub any container with stored water to remove possible eggs.
- Dress – Wear shoes, socks, long pants and long-sleeved shirts whenever you are outdoors to avoid mosquito bites.
- DEET – Apply insect repellent containing DEET, PICARDIN, IR3535, or oil of lemon eucalyptus according to manufacturer’s directions.
- Doors – Make sure doors and windows have tight-fitting screens. Repair or replace screens that have tears or holes to prevent mosquitos from entering your home.
- Report – If you notice small black and white mosquitoes in or around your home contact the San Bernardino County Department of Public Health, DEHS MVCP at (800) 442-2283.
Pertussis-related Resources
Pertussis – California Department of Public Health
Pertussis – Centers for Disease Control and Prevention
Pertussis (Whooping Cough)
What You Need to Know
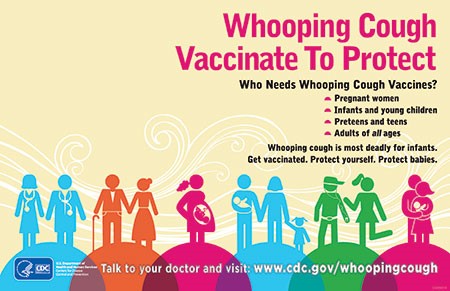
Whooping cough, known medically as pertussis, is a very contagious disease caused by a bacteria. It can cause serious illness in babies, children and adults. Babies are most at risk, because they are too young to be fully vaccinated.
Symptoms
The disease usually starts with cold-like symptoms and maybe a mild cough or fever. Symptoms of pertussis usually develop within 5 to 10 days after being exposed, but sometimes not for as long as 3 weeks. People with pertussis have severe coughing attacks that can last for months. As the disease progresses, the traditional symptoms of pertussis may appear and include many rapid coughs followed by a high-pitched “whoop”, throwing up during or after coughing fits and exhaustion following a coughing fit.
In babies, the cough can be minimal or not even there. Babies may have a symptom known as “apnea.” Apnea is a pause in the child’s breathing pattern. Babies too young for vaccination are at greatest risk for life-threatening cases of pertussis. In babies younger than 1 year old who get pertussis, about half need care in the hospital. The younger the baby, the more likely treatment in the hospital will be needed.
How Pertussis Spreads
Whooping cough (pertussis) is most contagious before the coughing starts. People with pertussis can spread the disease by coughing or sneezing while in close contact with others, who then breathe in the pertussis bacteria. Many babies are infected by parents, older siblings, or other caregivers who might not even know they have the disease.
Pertussis In California
There were 4,705 cases of pertussis with onset in 2015 reported to the California Department of Public Health, for a rate of 12.3 cases per 100,000 population. This includes 271 hospitalizations; 70 (26%) of these required intensive care. Of those hospitalized, 179 (66%) were infants younger than four months of age. Of those with pertussis onset in 2015, there were two deaths: one was a baby that was less than three weeks of age at the time of disease onset, and the other was an elderly woman with underlying health problems. (CDPH Pertussis Report dated June 27, 2016.)
Public Health Clinics in San Bernardino County
Pertussis vaccine is available at County Public Health Clinics. To make an appointment call 1 (800) 722-4777.
How To Prevent Pertussis
The best way to prevent pertussis (whooping cough) among babies, children, teens, and adults is to get vaccinated. Also, keep babies and other people at high risk for pertussis complications away from infected people. There are two vaccines used in the United States to help prevent whooping cough: DTaP and Tdap. These vaccines also provide protection against tetanus and diphtheria. Children younger than 7 years old get DTaP, while older children and adults get Tdap. Babies should begin their DTaP series by 2 months of age.
Pertussis Immunization Requirements for Child Care or Preschool
Pertussis Immunization Requirements for Grades TK/K-12
A single dose of Tdap is recommended for:
- Children and teens 11 through 18 years of age
- Adults 19 years of age and older
- Children 7-10 years of age who are not fully vaccinated against pertussis
- Pregnant women
The Centers for Disease Control and Prevention recommends pregnant women get a Tdap vaccine between the 27th and 36th week of each pregnancy, to create protective antibodies that pass to the baby before birth. These antibodies provide the baby some short-term protection against whooping cough in early life when the baby is too young to get vaccinated with DTaP.
Mumps
What Is Mumps?
Mumps is a contagious disease caused by a virus. The virus that causes Mumps primarily affects the parotid glands — one of three pairs of saliva-producing (salivary) glands, situated below and in front of your ears. Mumps is easily spread by airborne droplets from the upper respiratory tract.
What Are the Symptoms?
Mumps is best known for the puffy cheeks and swollen jaws that it causes. This is a result of swollen salivary glands. The most common symptoms include:
- Fever
- Headache
- Muscle aches
- Tiredness
- Loss of Appetite
- Swollen and tender salivary glands under the ears on one or both sides (parotitis)
Symptoms typically appear 16-18 days after infection, but this period can range from 12-25 days after infection. Some people who get mumps have very mild or no symptoms, and often they do not know they have the disease. Most people with mumps recover completely in a few weeks.
How Do I Prevent Getting Mumps?
Mumps can be prevented with MMR vaccine. This protects against three diseases: measles, mumps, and rubella. CDC recommends children get two doses of MMR vaccine, starting with the first dose at 12 through 15 months of age, and the second dose at 4 through 6 years of age. Teens and adults, who do not have evidence of immunity, should also be up-to-date on their MMR vaccination.
Children may also get MMRV vaccine, which protects against measles, mumps, rubella, and varicella (chickenpox). This vaccine is only licensed for use in children who are 12 months through 12 years of age.
Mumps on College Campuses